How to combat chronic inflammation
Why does chronic inflammation occur, and how can it be prevented? Lifestyle factors are key, including eating a healthy diet.

June 08, 2023
15 min read
Key takeaways
- Chronic inflammation is a prolonged reaction of the immune system that may be harmful to health. It is generally considered a hallmark of aging.
- A prolonged inflammatory state may be triggered by lifestyle factors such as a poor diet, insufficient physical activity, or poor quality sleep.
- Potential strategies to prevent chronic inflammation include consuming a diet rich in whole foods, calorie restriction, and fasting, as well as being physically active.
- Healthy functioning of the mitochondria, as well as the removal of damaged cells, known as autophagy, are both important for the prevention of chronic inflammation.
Chronic inflammation’s effect on the human body
Chronic inflammation is one of the hallmarks of aging, and addressing it through lifestyle factors is key when it comes to maintaining health with age. There are numerous strategies that may be used to combat this, and many involve diet and exercise. Promoting the health of the cells, including the mitochondria, is also a key part of addressing chronic inflammation, and this article will explain how.

What is chronic inflammation?
Inflammation is the body’s response to injury and infection and, as such, is a normal part of how we function. However, inflammation may occur in healthy tissues or last longer than normal, and this state of chronic inflammation may be harmful to health.[1]
Chronic inflammation is long-lasting inflammation that can go on for months or even years. Oftentimes, there may be elevated blood levels of different proinflammatory markers, as well as harmful changes inside the cell.[2]
Because of this, targeting chronic inflammation can be a key strategy for promoting health.
Symptoms of chronic inflammation
Chronic inflammation is associated with numerous chronic conditions, such as cardiovascular disease, chronic kidney disease, and Alzheimer’s disease. There may also be a decline in immune function associated with inflammation.[3]
Symptoms of chronic inflammation include:[4]
- Muscle and body pain
- Fatigue
- Mood changes, including depression and anxiety
- Gastrointestinal concerns
- Changes in weight
- Frequent infections
Symptoms of chronic inflammation could be signs of serious illness, so it’s important to check with your healthcare provider if you are experiencing any of these concerns.
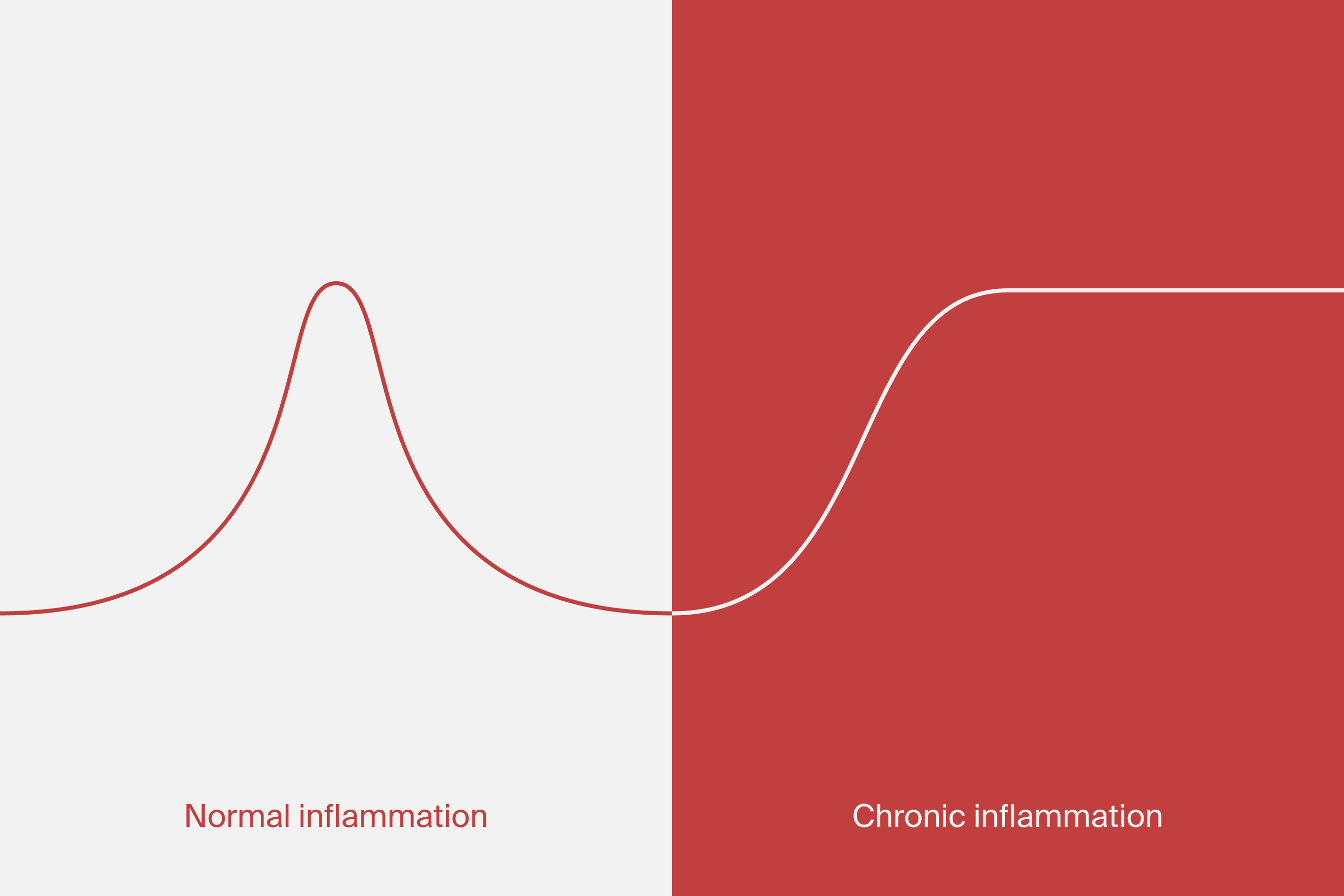
Difference between chronic and acute inflammation
Acute inflammation occurs in response to injury and infection and is short-lived. For example, this may occur when you cut your skin, and it turns red and swells.[5] This is a normal response of the immune system to keep the body healthy.
Chronic inflammation, in contrast, lasts longer than is needed and manifests in the body in harmful ways. A few things lead to chronic inflammation:[6]
- Unresolved infections from bacteria, fungi, and parasites that remain in the tissue for extended periods of time
- Exposure to environmental toxins like industrial chemicals
- Autoimmune conditions
- Defects in the cells responsible for mediating inflammation
- Multiple episodes of acute inflammation
- Increased production of free radicals and cellular debris from mitochondrial dysfunction and other oxidative stressors.
A number of factors may prevent acute inflammation from being halted at the appropriate time, and a state of persistent inflammation may occur. This activates the immune system in ways that are different from the acute reaction,[7] and it can have major effects on tissues and organs in the body, increasing disease risk.[8]

What causes chronic inflammation?
A number of risk factors for chronic inflammation have been identified, and these relate to lifestyle and social and physical environments.[9]
Diet
There are numerous dietary factors that have been linked to chronic inflammation.
Research suggests that a diet that lacks nutrient-dense whole foods such as fruits and vegetables and is high in ultra-processed foods may contribute to changes in the gut that may promote inflammation.
A diet with minimal whole foods lacks important vitamins and antioxidants to help resolve oxidative damage, while foods such as sugar, refined grains, and alcohol increase oxidative stress.[10]
Lack of physical activity
Physical inactivity has also been shown to be associated with chronic inflammation. Exercise reduces inflammation due to the release of certain proteins, and insufficient movement has been found to be related to higher levels of inflammatory markers. A link has also been found between inactivity and the risk for diseases associated with aging.[11]
Lifestyle-related factors
Among the other factors that may contribute to chronic inflammation are important lifestyle behaviors such as social interactions and sleep quality. Physical stressors at work in demanding environments may disrupt the body’s ability to down regulate inflammation at the appropriate time, potentially playing a role in disease.[12] Short sleep duration has also been implicated in chronic inflammation and the development of disease.[13]
Other factors
There are a number of other reasons chronic inflammation can occur, such as failure to eliminate an agent causing acute inflammation from the body. Examples of these are infectious organisms such as Mycobacterium tuberculosis, protozoa, fungi, and other parasites. The body may not be able to adequately defend itself against these microbes, so they may remain present for some time.[14]
Chronic inflammation’s role in aging
Inflammation that often occurs in people aged 50 or older is termed “inflammaging.”[15] As we age, there is an increase in pro-inflammatory markers and a high link to many age-related diseases. There is ongoing research seeking to understand the root causes of inflammaging, as well as the relationship between inflammaging and chronic diseases. Researchers are still trying to understand whether this type of inflammation causes disease or is simply an indicator of how fast biological aging is occurring.[16]
Recent research has explored how chronic inflammation can be addressed to promote healthy aging, and some of this research has focused on Urolithin A. Urolithin A can be made by the gut microbiome upon consumption of some foods but can also be taken in supplement form. It has been shown to have an anti-inflammatory effect and reduce inflammatory markers such as C-reactive protein (CRP), and it should be an important part of the discussion of how to promote healthy aging.[17]

How to prevent & reduce chronic inflammation
There are several ways to prevent or reduce chronic inflammation, including:
- Proper nutrition
- Taking specific supplements
- Calorie restriction and fasting
- Exercise
Sound nutrition has been highlighted as one way to prevent and reduce chronic inflammation. Particular dietary patterns, such as the Mediterranean diet, have been shown to be associated with lower levels of inflammatory markers that are considered hallmarks of inflammaging. Particular components of the diet, such as fruits and vegetables, whole grains, nuts, and fish, have also been found to be related to lower levels of inflammation.[18]
Specific nutrients have also been highlighted with respect to reducing chronic inflammation. For example, a high intake of dietary soluble and insoluble fiber is linked to a reduction in inflammatory markers. Micronutrients such as magnesium, vitamin D, vitamin E, zinc, and selenium are also considered anti-inflammatory.[19] Clinical trials with Mitopure (Urolithin A) have produced a reduction in inflammatory markers, including CRP, which may be important in reducing chronic inflammation.[20]
Calorie restriction (CR) is another dietary method that may potentially be used to prevent and reduce chronic inflammation. CR refers to an intake of daily calories below what is typical without resulting in malnutrition. It has been demonstrated that CR influences various processes in the body, including the inflammatory response and autophagy. Fasting has also been studied as an alternative to CR and may also produce similar effects. Fasting limits eating to a specific time window and may or may not produce a calorie deficiency, depending on the length of the fast. Additional research is needed to determine how the positive effects of CR and fasting may be derived without problems related to dietary restriction, such as malnutrition.[21]
Physical activity has also been touted as a method to prevent and reduce chronic inflammation. Exercise may decrease proinflammatory signals in the body, among numerous other benefits. The cardiovascular benefits of exercise also have been found to be related to a reduction in inflammation in vascular tissue, promoting healthy aging.[22]
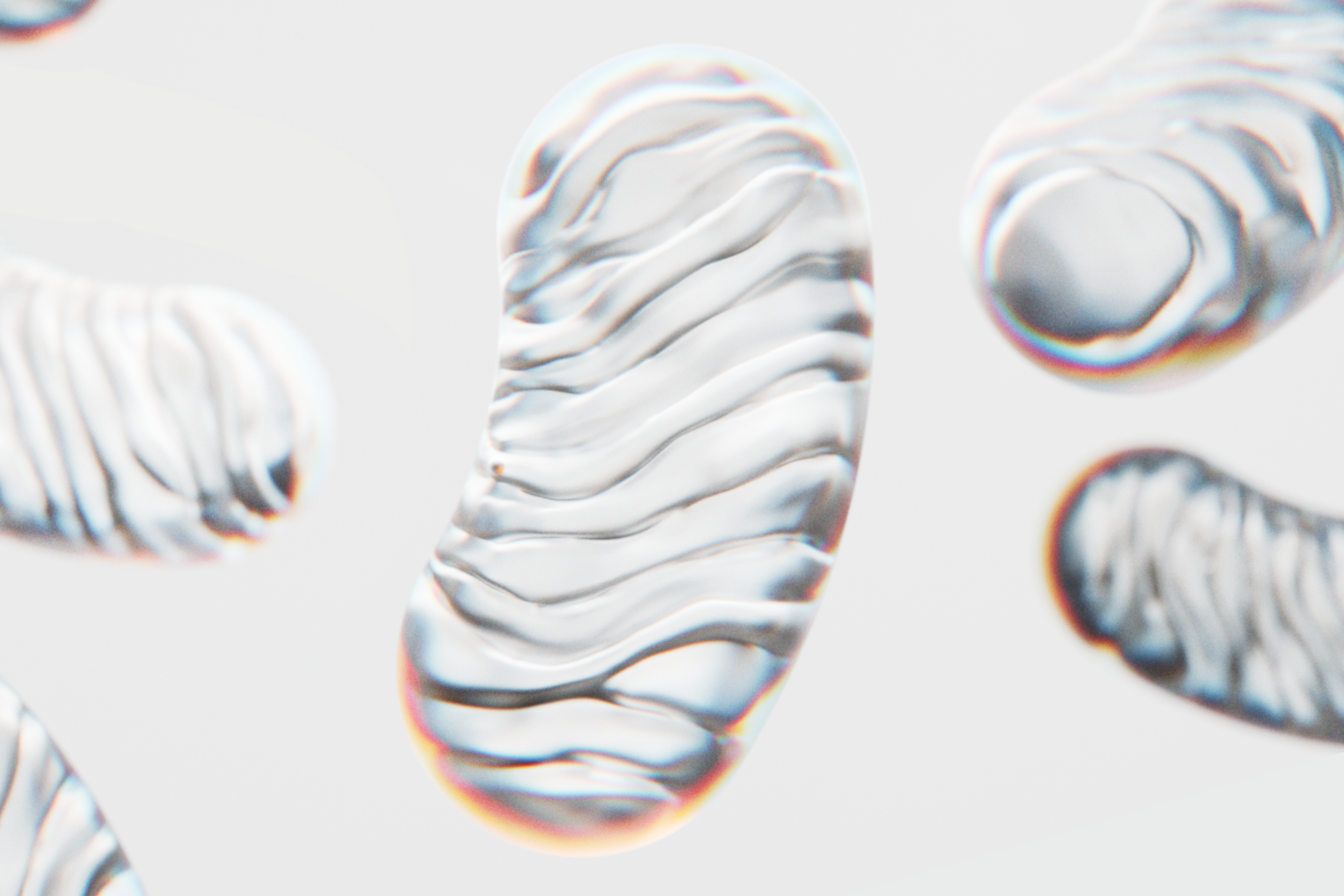
Mitochondrial dysfunction + inflammation
Mitochondria are considered the powerhouse of the cell, but when they become dysfunctional, they may promote inflammation. Mitochondrial function declines with age, and this may contribute to inflammation and cell death.[23] This decline in mitochondrial function has also been linked to chronic inflammatory conditions.[24]
Given the role of the mitochondria in the inflammatory response, they have also been identified as playing an important role in the immune response.[25] Changes in the dynamics in the mitochondria have been shown to be related to changes in immune function. There are numerous ways in which the mitochondria are involved in the immune response.[26]
Mitophagy and chronic inflammation
“Mitophagy” refers to the removal and recycling of damaged mitochondria and is necessary to maintain cellular function and disease prevention. [27]Mitophagy is linked to inflammation, as an impairment in this process results in inflammation and associated tissue damage. In short, with mitochondrial damage, you accumulate damaged mitochondria components. Without mitophagy, they are released in the cells and bloodstream, triggering an immune response and inflammation. Boosting mitophagy helps to clean these damage-associated signals and protect against the onset of inflammation.
Autophagy is an important part of the suppression of inflammaging, as a major function of autophagy is to inhibit proteins in the body that activate the inflammatory response.[28]It is involved in the functioning of the immune system, as well. This includes the body’s system of immune signaling, which is relevant to the development of inflammatory diseases. The impairment of autophagy can leave the body susceptible to such diseases.[29]
Urolithin A’s role in reducing inflammation
Urolithin A (UA) is a compound produced in the gut as a result of the consumption of antioxidants in foods such as pomegranates, berries, and walnuts.[30] UA has been well studied with respect to its role in promoting healthy aging.
UA works on the mitochondria of the cell by optimizing a process called mitophagy. As mitochondria become dysfunctional, the cells remove and recycle the damaged organelles, generating healthier and more efficient ones.
Another way that UA is involved in healthy aging relates to its anti-inflammatory effect. Early research demonstrated a decrease in levels of markers of inflammation with the administration of UA in rats.[33] In human trials, UA administration resulted in decreased levels of the inflammatory marker CRP.[32] It may impact inflammation in different ways depending on the tissues affected and condition, and additional studies in humans are needed to further explore this.[31]
Recent preclinical studies suggest that UA has an anti-inflammatory effect in various tissues, including the brain, adipose, heart, and liver tissues. Given this, it has been implicated in the prevention of conditions such as Alzheimer’s disease, type 2 diabetes mellitus, and non-alcoholic fatty liver disease.[34]
Urolithin A’s role in improving immune function
A number of preclinical trials have looked at UA’s role in improving immune function.
UA may work to enhance immune function.[35] It has also been shown to reduce oxidative stress in immune cells and attenuate inflammation. These roles relate to the functioning of the immune system.[36] Research exploring the role of UA has revealed its immunomodulating effects, including how it can support T memory cell expansion.[37]
T-memory cells are potent immune cells that play a role in the early targeting of pathogens and cancer cells. As we age, they become exhausted, reducing their ability to initiate an immune response. An important pre-clinical trial looking at mouse models demonstrated that by supplementing with UA, T memory cell function was improved by activating mitophagy, suggesting an important role that UA may play in immune health.[38]
UA’s role in improving immune function has also been examined with regard to particular chronic conditions in preclinical trials. For example, research focused on the therapeutic potential of UA to support cancer treatment and prevention highlighted the anti-inflammatory effects of UA, which may be of importance for preventing immune suppression associated with chronic inflammation in cancer.[39]
More research is needed in humans to fully understand how it may help in cancer prevention.
Final thoughts
Chronic inflammation and inflammaging are closely linked to many diseases of aging. By following a healthy diet, exercising regularly, getting plenty of sleep, and using targeted supplements like Mitopure, we may be able to improve inflammatory markers and slow down the development of age-related inflammation.
Disclaimer - The information in this article is for informational purposes only and should not be taken as medical advice. Always consult with your medical doctor for personalized medical advice.
References
- ↑
National Institute of Environmental Health Sciences. Inflammation. 2021. Accessed February 22, 2023. Available at https://www.niehs.nih.gov/health/topics/conditions/inflammation/index.cfm
- ↑
Ferrucci L, Fabbri E. Inflammaging: chronic inflammation in aging, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018 Sep;15(9):505-522. doi: 10.1038/s41569-018-0064-2. PMID: 30065258; PMCID: PMC6146930.
- ↑
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: An expanding universe. Cell. 2023 Jan 19;186(2):243-278. doi: 10.1016/j.cell.2022.11.001. Epub 2023 Jan 3. PMID: 36599349.
- ↑
Pahwa R, Goyal A, Jialal I. Chronic Inflammation. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493173/
- ↑
National Institute of Environmental Health Sciences. Inflammation. 2021. Accessed February 22, 2023. Available at https://www.niehs.nih.gov/health/topics/conditions/inflammation/index.cfm
- ↑
Pahwa R, Goyal A, Jialal I. Chronic Inflammation. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493173/
- ↑
Calder PC, Ahluwalia N, Albers R, Bosco N, Bourdet-Sicard R, Haller D, Holgate ST, Jönsson LS, Latulippe ME, Marcos A, Moreines J, M'Rini C, Müller M, Pawelec G, van Neerven RJ, Watzl B, Zhao J. A consideration of biomarkers to be used for evaluation of inflammation in human nutritional studies. Br J Nutr. 2013 Jan;109 Suppl 1:S1-34. doi: 10.1017/S0007114512005119. PMID: 23343744.
- ↑
Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the lifespan. Nat Med. 2019 Dec;25(12):1822-1832. doi: 10.1038/s41591-019-0675-0. Epub 2019 Dec 5. PMID: 31806905; PMCID: PMC7147972.
- ↑
Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the lifespan. Nat Med. 2019 Dec;25(12):1822-1832. doi: 10.1038/s41591-019-0675-0. Epub 2019 Dec 5. PMID: 31806905; PMCID: PMC7147972.
- ↑
Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the lifespan. Nat Med. 2019 Dec;25(12):1822-1832. doi: 10.1038/s41591-019-0675-0. Epub 2019 Dec 5. PMID: 31806905; PMCID: PMC7147972.
- ↑
Fiuza-Luces C, Santos-Lozano A, Joyner M, Carrera-Bastos P, Picazo O, Zugaza JL, Izquierdo M, Ruilope LM, Lucia A. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018 Dec;15(12):731-743. doi: 10.1038/s41569-018-0065-1. PMID: 30115967.
- ↑
Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences. 2012 Apr 17;109(16):5995-9.
- ↑
Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol. 2019 Apr;16(4):213-224. doi: 10.1038/s41569-018-0109-6. PMID: 30410106.
- ↑
Pahwa R, Goyal A, Jialal I. Chronic inflammation. StatPearls [Internet]. 2021 Sep 28.
- ↑
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G. Inflamm‐aging: an evolutionary perspective on immunosenescence. Annals of the New York Academy of Sciences. 2000 Jun;908(1):244-54.
- ↑
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G. Inflamm‐aging: an evolutionary perspective on immunosenescence. Annals of the New York Academy of Sciences. 2000 Jun;908(1):244-54.
- ↑
D’Amico D, Andreux PA, Valdés P, Singh A, Rinsch C, Auwerx J. Impact of the natural compound urolithin A on health, disease, and aging. Trends in molecular medicine. 2021 Jul 1;27(7):687-99.
Liu S, D’Amico D, Shankland E, et al. Effect of Urolithin A Supplementation on Muscle Endurance and Mitochondrial Health in Older Adults: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(1):e2144279. doi:10.1001/jamanetworkopen.2021.44279
- ↑
Di Giosia P, Stamerra CA, Giorgini P, Jamialahamdi T, Butler AE, Sahebkar A. The role of nutrition in inflammaging. Ageing Res Rev. 2022 May;77:101596. doi: 10.1016/j.arr.2022.101596. Epub 2022 Feb 24. PMID: 35219904.
- ↑
Pahwa R, Goyal A, Jialal I. Chronic inflammation. StatPearls [Internet]. 2021 Sep 28.
- ↑
Liu S, D’Amico D, Shankland E, et al. Effect of Urolithin A Supplementation on Muscle Endurance and Mitochondrial Health in Older Adults: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(1):e2144279. doi:10.1001/jamanetworkopen.2021.44279
- ↑
Di Giosia P, Stamerra CA, Giorgini P, Jamialahamdi T, Butler AE, Sahebkar A. The role of nutrition in inflammaging. Ageing Res Rev. 2022 May;77:101596. doi: 10.1016/j.arr.2022.101596. Epub 2022 Feb 24. PMID: 35219904.
- ↑
Di Giosia P, Stamerra CA, Giorgini P, Jamialahamdi T, Butler AE, Sahebkar A. The role of nutrition in inflammaging. Ageing Res Rev. 2022 May;77:101596. doi: 10.1016/j.arr.2022.101596. Epub 2022 Feb 24. PMID: 35219904.
- ↑
Amorim JA, Coppotelli G, Rolo AP, Palmeira CM, Ross JM, Sinclair DA. Mitochondrial and metabolic dysfunction in ageing and age-related diseases. Nature Reviews Endocrinology. 2022 Apr;18(4):243-58.
- ↑
Naik E, Dixit VM. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J Exp Med. 2011 Mar 14;208(3):417-20. doi: 10.1084/jem.20110367. Epub 2011 Feb 28. PMID: 21357740; PMCID: PMC3058577.
- ↑
Missiroli S, Genovese I, Perrone M, Vezzani B, Vitto VAM, Giorgi C. The Role of Mitochondria in Inflammation: From Cancer to Neurodegenerative Disorders. J Clin Med. 2020 Mar 9;9(3):740. doi: 10.3390/jcm9030740. PMID: 32182899; PMCID: PMC7141240.
- ↑
Mohanty A, Tiwari-Pandey R, Pandey NR. Mitochondria: the indispensable players in innate immunity and guardians of the inflammatory response. J Cell Commun Signal. 2019 Sep;13(3):303-318. doi: 10.1007/s12079-019-00507-9. Epub 2019 Feb 4. PMID: 30719617; PMCID: PMC6732146.
- ↑
Tabibzadeh S. Role of autophagy in aging: The good, the bad, and the ugly. Aging Cell. 2023 Jan;22(1):e13753. doi: 10.1111/acel.13753. Epub 2022 Dec 20. PMID: 36539927; PMCID: PMC9835585.
Shintani, T. , & Klionsky, D. J. (2004). Autophagy in health and disease: A double‐edged sword. Science, 306(5698), 990–995.
- ↑
Aman Y, Schmauck-Medina T, Hansen M, Morimoto RI, Simon AK, Bjedov I, Palikaras K, Simonsen A, Johansen T, Tavernarakis N, Rubinsztein DC, Partridge L, Kroemer G, Labbadia J, Fang EF. Autophagy in healthy aging and disease. Nat Aging. 2021 Aug;1(8):634-650. doi: 10.1038/s43587-021-00098-4. Epub 2021 Aug 12. PMID: 34901876; PMCID: PMC8659158.
- ↑
Matsuzawa-Ishimoto Y, Hwang S, Cadwell K. Autophagy and inflammation. Annual review of immunology. 2018 Apr 26;36:73-101.
- ↑
D’Amico D, Andreux PA, Valdés P, Singh A, Rinsch C, Auwerx J. Impact of the natural compound urolithin A on health, disease, and aging. Trends in molecular medicine. 2021 Jul 1;27(7):687-99.
- ↑
D’Amico D, Andreux PA, Valdés P, Singh A, Rinsch C, Auwerx J. Impact of the natural compound urolithin A on health, disease, and aging. Trends in molecular medicine. 2021 Jul 1;27(7):687-99.
- ↑
Liu S, D’Amico D, Shankland E, et al. Effect of Urolithin A Supplementation on Muscle Endurance and Mitochondrial Health in Older Adults: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(1):e2144279. doi:10.1001/jamanetworkopen.2021.44279
- ↑
Larrosa M, González-Sarrías A, Yáñez-Gascón MJ, Selma MV, Azorín-Ortuño M, Toti S, Tomás-Barberán F, Dolara P, Espín JC. Anti-inflammatory properties of a pomegranate extract and its metabolite urolithin-A in a colitis rat model and the effect of colon inflammation on phenolic metabolism. J Nutr Biochem. 2010 Aug;21(8):717-25. doi: 10.1016/j.jnutbio.2009.04.012. Epub 2009 Jul 18. PMID: 19616930.
- ↑
Toney AM, Fox D, Chaidez V, Ramer-Tait AE, Chung S. Immunomodulatory Role of Urolithin A on Metabolic Diseases. Biomedicines. 2021 Feb 15;9(2):192. doi: 10.3390/biomedicines9020192. PMID: 33671880; PMCID: PMC7918969.
- ↑
Larrosa M, González-Sarrías A, Yáñez-Gascón MJ, Selma MV, Azorín-Ortuño M, Toti S, Tomás-Barberán F, Dolara P, Espín JC. Anti-inflammatory properties of a pomegranate extract and its metabolite urolithin-A in a colitis rat model and the effect of colon inflammation on phenolic metabolism. J Nutr Biochem. 2010 Aug;21(8):717-25. doi: 10.1016/j.jnutbio.2009.04.012. Epub 2009 Jul 18. PMID: 19616930.
- ↑
Toney AM, Fox D, Chaidez V, Ramer-Tait AE, Chung S. Immunomodulatory Role of Urolithin A on Metabolic Diseases. Biomedicines. 2021 Feb 15;9(2):192. doi: 10.3390/biomedicines9020192. PMID: 33671880; PMCID: PMC7918969.
- ↑
Piwowarski J.P., Granica S., Kiss A.K. Influence of gut microbiota-derived ellagitannins’ metabolites urolithins on pro-inflammatory activities of human neutrophils. Planta Med. 2014;80:887–895. doi: 10.1055/s-0034-1368615.
Denk D, Petrocelli V, Conche C, Drachsler M, Ziegler PK, Braun A, Kress A, Nicolas AM, Mohs K, Becker C, Neurath MF, Farin HF, Buchholz CJ, Andreux PA, Rinsch C, Greten FR. Expansion of T memory stem cells with superior anti-tumor immunity by Urolithin A-induced mitophagy. Immunity. 2022 Nov 8;55(11):2059-2073.e8. doi: 10.1016/j.immuni.2022.09.014. Epub 2022 Oct 19. PMID: 36351375.
- ↑
Denk D, Petrocelli V, Conche C, Drachsler M, Ziegler PK, Braun A, Kress A, Nicolas AM, Mohs K, Becker C, Neurath MF, Farin HF, Buchholz CJ, Andreux PA, Rinsch C, Greten FR. Expansion of T memory stem cells with superior anti-tumor immunity by Urolithin A-induced mitophagy. Immunity. 2022 Nov 8;55(11):2059-2073.e8. doi: 10.1016/j.immuni.2022.09.014. Epub 2022 Oct 19. PMID: 36351375.
- ↑
Rønning SB, Voldvik V, Bergum SK, Aaby K, Borge GIA. Ellagic acid and urolithin A modulate the immune response in LPS-stimulated U937 monocytic cells and THP-1 differentiated macrophages. Food Funct. 2020 Sep 23;11(9):7946-7959. doi: 10.1039/c9fo03008e. PMID: 32832941.
Authors
Jinan Banna
Writter
Reviewed by
Jen Scheinman